Rethink the links between genes and disease
The rethink on pathogenicity shows that researchers who hunt for genetic mutations likely to cause disease need to be cautious. Many, it seems, have not required enough evidence before asserting that a particular variant is harmful.
Rethink the links between genes and disease
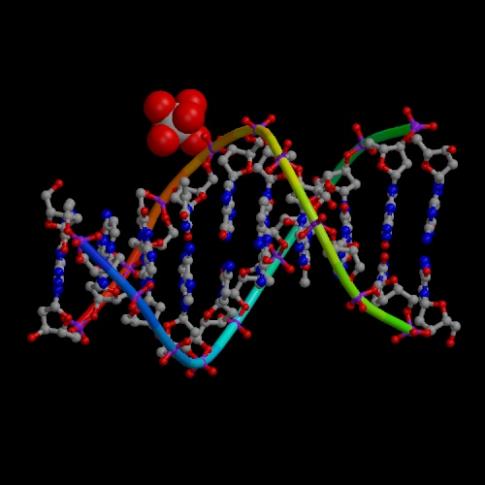
The ExAC database has shown that many mutations thought to be harmful are benign.
One of the major findings of the Exome Aggregation Consortium (ExAC), the largest-ever catalogue of genetic variation in the protein-coding regions of the human genome, is that many genetic mutations have been misclassified as harmful (M. Lek et al. Nature 536, 285–291; 2016). Authors of that study estimate that each person has lurking in their genome an average of 54 mutations that are currently considered pathogenic — but that about 41 of these occur so frequently in the human population that they aren’t in fact likely to cause severe disease. That finding is having major consequences for some people with such variants, lifting the equivalent of genetic death sentences.
That raises two challenges for researchers: how to sort out which mutations currently considered pathogenic are actually benign, and how to apply more rigorous tests to future research that aims to find the genetic causes of disease.
Working out which mutations are actually linked to illness will be a long and arduous task. For instance, geneticist and physician Leslie Biesecker of the US National Human Genome Research Institute in Bethesda, Maryland, found that a patient referred to him for diagnosis harboured a genetic variant that had been linked to kidney failure. Yet it turned out that the variant was too common in ExAC to realistically be causing a rare kidney ailment. So Biesecker checked genome sequences from 950 people whom he had previously sequenced in a study called ClinSeq (K. L. Lewis et al. PLoS ONE 10, e0132690; 2015). Five of them had the same variant, with no history of kidney disease, indicating that the variant probably does not actually cause this illness. To probe further, Biesecker is now recontacting the five ClinSeq participants with the variant to ask them to take part in follow-up tests to check whether they have normal kidney function, including collecting multiple urine samples over a 24-hour period.
To reassess the links between diseases and mutations, researchers must have access to a group of people whose detailed genetic and clinical information are known, and that’s rare. It also takes time and some cost; multiply that by the huge numbers of ‘pathogenic’ variants that have been called into question, and researchers are looking at a major undertaking. It’s a crucial one, because geneticists are being asked every day to make judgements about the harm that could be caused by mutations found in patients’ genomes. Biesecker hopes that planned or existing projects to link people’s genomes to their detailed health records — such as the US president’s Precision Medicine Initiative, which aims to sequence at least 1 million Americans, and the UK 100,000 Genomes Project — will help.
“Many have not required enough evidence before asserting that a particular variant is harmful.”
The rethink on pathogenicity shows that researchers who hunt for genetic mutations likely to cause disease need to be cautious. Many, it seems, have not required enough evidence before asserting that a particular variant is harmful.
Early efforts to discover the genetic underpinnings of disease started with families in which a particular condition recurred, generation after generation. By studying their extensive pedigrees, researchers could see strong evidence that certain mutations caused the disease. But in recent years, researchers have switched tactics: for instance, searching for evidence of pathogenicity by scanning for mutations that are more common in people with disease than in those without. It is becoming clear that many human genetic variations are relatively rare, and when researchers do not examine large enough groups of people with and without disease when scanning for pathogenic mutations, they are likely to mistakenly conclude that particular variants of interest turn up only in people with disease. The truth may be that they just haven’t looked hard enough for these variants elsewhere.
These conclusions have consequences for real people, and so researchers must go about this work differently. When they suspect that a variant is linked to disease, they should check to see how common it is in databases such as ExAC. Even better, they should hunt for evidence that the mutation has a functional role in disease before declaring that it is pathogenic. Let the reckoning begin.
One of the major findings of the Exome Aggregation Consortium (ExAC), the largest-ever catalogue of genetic variation in the protein-coding regions of the human genome, is that many genetic mutations have been misclassified as harmful (M. Lek et al. Nature 536, 285–291; 2016). Authors of that study estimate that each person has lurking in their genome an average of 54 mutations that are currently considered pathogenic — but that about 41 of these occur so frequently in the human population that they aren’t in fact likely to cause severe disease. That finding is having major consequences for some people with such variants, lifting the equivalent of genetic death sentences.
That raises two challenges for researchers: how to sort out which mutations currently considered pathogenic are actually benign, and how to apply more rigorous tests to future research that aims to find the genetic causes of disease.
Working out which mutations are actually linked to illness will be a long and arduous task. For instance, geneticist and physician Leslie Biesecker of the US National Human Genome Research Institute in Bethesda, Maryland, found that a patient referred to him for diagnosis harboured a genetic variant that had been linked to kidney failure. Yet it turned out that the variant was too common in ExAC to realistically be causing a rare kidney ailment. So Biesecker checked genome sequences from 950 people whom he had previously sequenced in a study called ClinSeq (K. L. Lewis et al. PLoS ONE 10, e0132690; 2015). Five of them had the same variant, with no history of kidney disease, indicating that the variant probably does not actually cause this illness. To probe further, Biesecker is now recontacting the five ClinSeq participants with the variant to ask them to take part in follow-up tests to check whether they have normal kidney function, including collecting multiple urine samples over a 24-hour period.
To reassess the links between diseases and mutations, researchers must have access to a group of people whose detailed genetic and clinical information are known, and that’s rare. It also takes time and some cost; multiply that by the huge numbers of ‘pathogenic’ variants that have been called into question, and researchers are looking at a major undertaking. It’s a crucial one, because geneticists are being asked every day to make judgements about the harm that could be caused by mutations found in patients’ genomes. Biesecker hopes that planned or existing projects to link people’s genomes to their detailed health records — such as the US president’s Precision Medicine Initiative, which aims to sequence at least 1 million Americans, and the UK 100,000 Genomes Project — will help.
“Many have not required enough evidence before asserting that a particular variant is harmful.”
The rethink on pathogenicity shows that researchers who hunt for genetic mutations likely to cause disease need to be cautious. Many, it seems, have not required enough evidence before asserting that a particular variant is harmful.
Early efforts to discover the genetic underpinnings of disease started with families in which a particular condition recurred, generation after generation. By studying their extensive pedigrees, researchers could see strong evidence that certain mutations caused the disease. But in recent years, researchers have switched tactics: for instance, searching for evidence of pathogenicity by scanning for mutations that are more common in people with disease than in those without. It is becoming clear that many human genetic variations are relatively rare, and when researchers do not examine large enough groups of people with and without disease when scanning for pathogenic mutations, they are likely to mistakenly conclude that particular variants of interest turn up only in people with disease. The truth may be that they just haven’t looked hard enough for these variants elsewhere.
These conclusions have consequences for real people, and so researchers must go about this work differently. When they suspect that a variant is linked to disease, they should check to see how common it is in databases such as ExAC. Even better, they should hunt for evidence that the mutation has a functional role in disease before declaring that it is pathogenic. Let the reckoning begin.
* * *
Scientific buzzwords obscure meaning
‘Nexus’ is enjoying new-found popularity. But what does it actually mean?
In the twenty-first century, the term nexus stands for more than its dictionary definition of a connection or focus point. It’s a buzzword, especially when tagged on to the end of a string of associated nouns.
For example, an article in Environmental Science and Policy this month draws attention to the popularization of the phrase ‘water–energy–food nexus’ in debates over the use of natural resources (R. Cairns and A. Krzywoszynska Environ. Sci. Policy 64, 164–170; 2016).
Language matters and, although Aaron Ellison argues in this week’s World View on page 141 that the term “natural resources” itself should be retired, we’ll skip that to examine Cairns and Krzywoszynska’s main point: buzzwords are Orwellian and obfuscate even as they pretend to enlighten. Discussions of the nexus between connected crises, in other words, can generate more linguistic heat than policy light.
The authors argue that “understandings and usage of the term nexus are plural, fragmented and ambiguous”. This is not always viewed as a negative by those who use the word, of course. When there is little of substance to say, it often helps to use language that acts as a mirror so finely polished that every reader can see their own agenda and interests reflected. There are echoes here of the way the term Anthropocene has been adopted and borrowed by a range of scientific disciplines, each of which wants a taste of the action.
“The term nexus appears to have something of a paradoxical quality,” say Cairns and Krzywoszynska, “being simultaneously unarguably true at a simple descriptive level, and yet confusingly unintelligible or meaningless to actors unfamiliar with the discourse.”
The motives behind the eagerness to jump on the nexus bandwagon are not always sinister. Honest brokers use the term to try to encapsulate that unspoken and undefined territory where the implications of one action bleed into another; when the equal and opposite reaction also has consequences.
But the risk is that containing this territory, however loosely, constrains it instead — and that the nexus becomes the focus of the analysis, rather than a natural consequence of studying the supporting problems.
Perhaps, like the most distant stars, the nexus is best viewed only with peripheral vision: we can see it’s there, but we shouldn’t focus our gaze directly on it lest its true nature slips from view. And, at the very least, it shows that we should choose our buzzwords with care. /Nature




 del.icio.us
del.icio.us Digg
Digg

Post your comment